When Prescribed Medication and Genetics Are a Mismatch, It Can Prove Fatal
A Team of NYU Dual-Degree Students Came Up with an Award-Winning Solution

(L to R) Yazn Alzeghaib, Adam Almaktari, James Gerber (CFO Presage), Muhammad Zain Naveed, Haris Sahmanovic
Muhammad Zain Naveed was still in high school when a close friend back in Pakistan died after taking a medication that should have helped him. The drug was standard, the dosage was normal, and the outcome was preventable — but only in hindsight, once doctors understood that their patient's genetic makeup had made the treatment inappropriate for him.
That loss stayed with Zain, and it led to a question he couldn't shake: why does modern medicine still treat everyone the same when our DNA makes us fundamentally different from one another?
Recently, competing at Hack@Brown — one of the nation's most selective collegiate hackathons — Zain and his teammates tackled that question. Their application, dubbed MedGuard, won the "Best Use of Presage" award, recognizing the most innovative use of the company’s real-time physiological monitoring technology, which turns any cell-phone camera into a health-monitoring device.
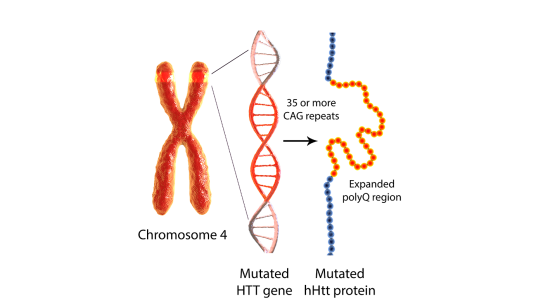
MedGuard works by combining two kinds of data that medical practitioners have rarely brought together: a patient's genomic profile and live signals from their own body. Using data from consumer genomics services, MedGuard identifies patients who carry genetic variants that affect how they metabolize certain drugs. Patients with genetic variants that impair drug-metabolizing enzymes can reach toxic medication levels in the bloodstream at standard doses. Because these gene-drug interactions are often asymptomatic initially, dangerous side effects may develop without warning.
Zain is particularly attuned to this problem because the populations most affected are often the least represented in medical research. Most pharmacogenomic studies have been conducted predominantly on patients of European descent, leaving people of South Asian, African, and other backgrounds with less reliable data about how drugs will work for them. Conditions like Thalassemia and Sickle Cell — more prevalent in South Asian populations — can compound these risks in ways that mainstream clinical guidelines may not fully account for.
What makes MedGuard distinctive is its ability to catch the danger in real time, before a patient reaches the hospital. Zain’s team used the Presage application programming interface (API) to transform an ordinary smartphone into a passive physiological monitor, with no external hardware required. By analyzing micro-movements captured by the phone's accelerometer and gyroscope, MedGuard can detect subtle signs of drug toxicity — faint tremors, slight motor instability, or changes in movement signature that precede a full adverse reaction. When a patient's genomic profile suggests high metabolic risk, and the phone simultaneously detects these physical signals, MedGuard issues an alert. The "double lock" design is intentional: either signal alone might mean nothing, but both together indicate real danger.
The problem MedGuard is targeting is not rare. Each year in the United States, adverse drug reactions send an estimated two million people to the hospital and contribute to more than 200,000 deaths — making them a major cause of preventable mortality. The standard approach remains largely trial-and-error: prescribe, observe, adjust. For patients with genetic vulnerabilities that haven't been identified or communicated to their doctors, that process can be fatal.
"We successfully demonstrated how undergraduate students can solve complex clinical problems by combining bioinformatics, mobile computing, and heuristic algorithmic logic," Zain wrote, describing the project, and the Hack@Brown judges agreed – as did Presage executives, who were in attendance at the competition and confirmed MedGuard’s potential marketability.
For Zain, the recognition is meaningful — but it's secondary to what the technology could eventually do. His friend in Pakistan didn't have to die, and neither did the hundreds of thousands of other people who lose their lives each year due to adverse drug interactions. MedGuard may be an undergraduate project today, but it could one day be in the hands of clinicians and patients.
Dual Power
The NYU team that built MedGuard reflects the kind of collaboration Tandon has long worked to cultivate. Muhammad Zain Naveed is a student in a dual-degree, pre-med program that spans both Tandon and the College of Arts and Sciences, and he is president of the Hemmes Engineering and Science Society (HESS), an arm of NYU's Dual-Degree Engineering program.
He met his teammates — Adam Almaktari, Yazn Alzeghaibi, and Haris Sahmanovic, who are all Tandon students — in that capacity. That combination matters: the problem MedGuard addresses requires fluency in both the underlying biology and the engineering required to act on it, and the team members, as they’ve shown, have both.