Pathways to Understand Drug Delivery in the Treatment of Arthritis

Speaker:
Lori A. Setton, PhD
Lucy and Stanley Lopata Distinguished Professor
Chair of Biomedical Engineering, Washington University
Abstract:
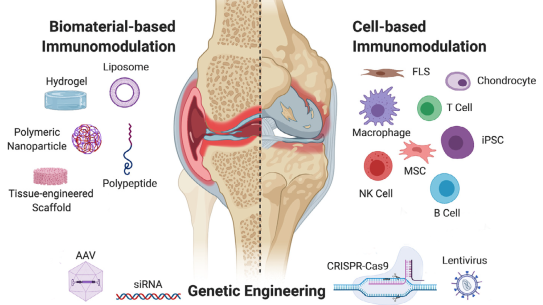
Research and development have advanced the clinical use of protein and small-molecule drugs that can modify the progression and symptoms of osteoarthritis and inflammatory pain, including mediators of TNF-alpha and the NF-kappa B pathway. Systemic administration of these drugs can have serious side effects that motivate the employment of local drug delivery strategies, such as intra-articular injection, to prolong drug residence time and decrease serum exposure. Our laboratory both develops in situ forming drug depots for sustained drug delivery to the joint over time and constructs computational models of drug clearance to understand governing processes. Here we will review the synthesis and design of intra-articular drug depots, and show evidence that drugs retain substantial bioactivity and disease-modifying effects in vivo. We further describe our ex vivo models to advance an understanding of factors affecting drug transport in the joint space towards the goal of designing optimal drug delivery strategies.
Prof. Setton received her BSE from Princeton University and MS and PhD degrees in Mechanical Engineering from Columbia University. She joined Duke University in 1994, where she served as the Bevan Professor of Biomedical Engineering and Orthopaedic Surgery before becoming the Chair of the Dept. of Biomedical Engineering at Washington University in 2015. Prof. Setton is a Fellow of the BMES, ASME, ORS, and AIMBE, has served as President of the Biomedical Engineering Society, and received a PECASE Award, Christopher Jacobs Award for Excellence in Leadership, Graduate Dean's Award for Excellence in Mentoring, and ASME’s Mow Medal and Lissner Medal.